Three cabinet-level federal departments found that health plans are failing to ensure mental health parity in their benefit plans.
The U.S. Labor Department, Health and Human Services Department and Department of the Treasury issued a 54-page report today spelling out how group health plans or health insurance issuers have fallen short of their legal obligations to ensure that financial requirements and treatment limitations aren’t more restrictive than those that apply to medical and surgical benefits.
The report is meant to highlight the departments’ increased vigor in enforcing mental health parity laws and rules.
Behavioral health groups have long sought for mental health parity within payers’ benefits and thought they achieved a key victory with the passage of the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA). However, the law was not actively enforced and more recent actions by the Biden administration have sought to correct that.
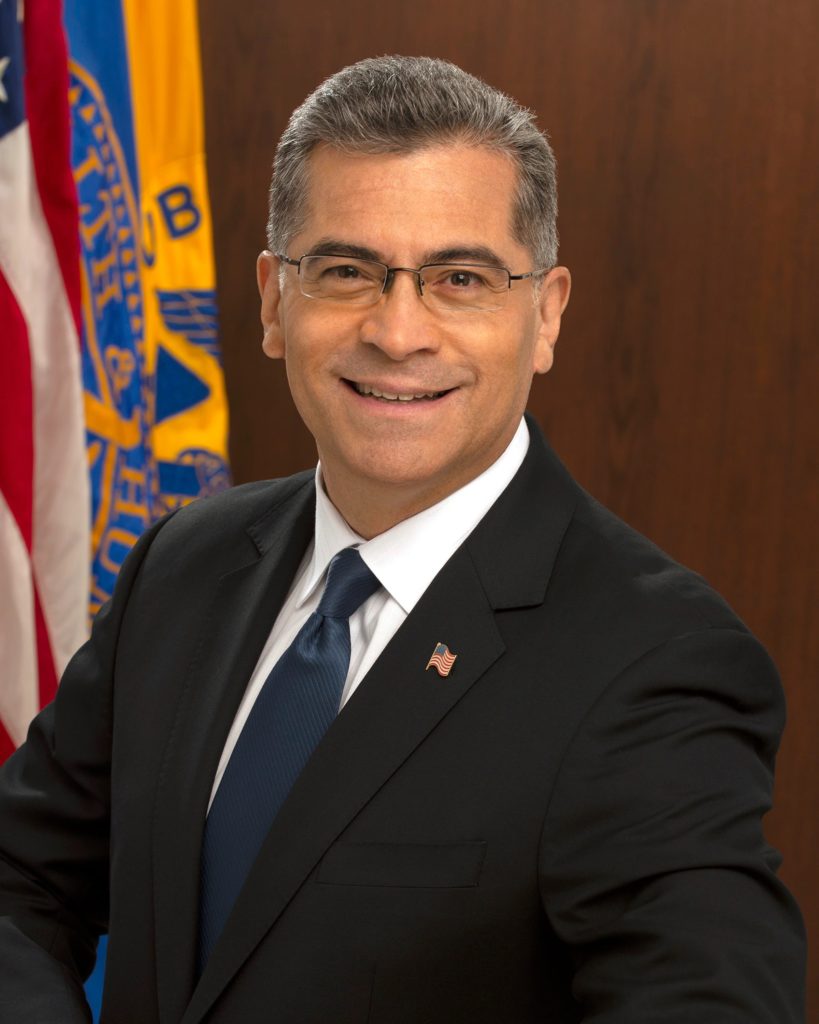
“Access to mental and behavioral health support is critical as the COVID-19 pandemic continues to impact so many lives across the country,” U.S. Secretary of Health and Human Services Xavier Becerra said in a news release. “Unfortunately, as today’s report shows, health plans and insurance companies are falling short of providing access to the treatment many working families need. We are committed to working with our federal partners to change this and hold health plans and insurance companies accountable for delivering more comprehensive care.”
The MHPAEA was amended by the Consolidated Appropriations Act of 2021 to strengthen mental health parity enforcement.
The Department of Labor’s Employee Benefits Security Administration (EBSA) is taking “unprecedented steps” to enforce the MHPAEA, the release states. Also, it states that the Centers for Medicare & Medicaid Services (CMS), a part of the Health and Human Services Department, has increased its MHPAEA enforcement activities in the individual and fully insured group markets in states where CMS has enforcement authority and over non-federal governmental plans in all states.
The report states that the EBSA has issued 156 letters within 86 investigations seeking more information about non-quantitative treatment limitations, or practices that limit access to care that aren’t numerically based like prior authorizations. None of the initial responses from the payers contain sufficient information to assess them for mental health parity, the report states.
Of the information that departments have received, some key themes include — to name just a few — a lack of meaningful comparison or meaningful analysis of the treatment limitations; limiting the information to a portion of treatment limitations at issue; and failure to show that the limitation complies with regulatory standards.
“The report’s findings clearly indicate that health plans and insurance companies are falling short of providing parity in mental health and substance-use disorder benefits, at a time when those benefits are needed like never before,” U.S. Secretary of Labor Marty Walsh said in the release. “The pandemic is having a negative impact on the mental health of people in the U.S. and driving a rise in substance use. As a person in recovery, I know firsthand how important access to mental health and substance-use disorder treatment is. Enforcement of this law is a top priority for the Department of Labor and an objective I take personally.”
Companies featured in this article:
U.S. Department of Health and Human Services, U.S. Department of the Treasury, U.S. Health and Human Services Department, U.S. Labor Department