Providers approved for the U.S. Centers for Medicare & Medicaid Services’ (CMS) new ACO REACH program are seeing an opportunity to further integrate behavioral health into care.
Earlier this year, CMS announced it was nixing direct contracting and replacing it with the ACO Realizing Equity, Access and Community Health (REACH) model. Multiple direct-contracting models were unveiled under the previous CMS administration, but Biden officials opted to scrap them after a wave of backlash from health care stakeholders.
Like other Accountable Care Organizations (ACOs), the REACH model ties provider reimbursement to quality metrics. The defining feature of an ACO REACH is a focus on equity, access and care coordination, including to those in traditionally underserved communities.
Now, some providers are seeing this as a catalyst to incorporating innovative behavioral health services into care.
CMS previously noted that participants formerly under the direct-contracting models offered a variety of services, including preventive behavioral health services, for underserved populations. The agency is encouraging this strategy for the future under REACH as well.
“Under the ACO REACH Model, health care providers can receive more predictable revenue and use those dollars more flexibly to meet their patients’ needs — and to be more resilient in the face of health challenges like the current public health pandemic,” CMS Deputy Administrator and CMS Innovation Center Director Liz Fowler said when REACH was first announced. “The bottom line is that ACOs can improve health care quality and make people healthier, which can also lead to lower total costs of care.”
In addition to its focus on health equity, REACH’s design also includes policies to ensure doctors and other health care providers play a primary role in accountable care. At least 75% control of each ACO’s governing body must be held by participating providers or their designated representatives.
Making the cut
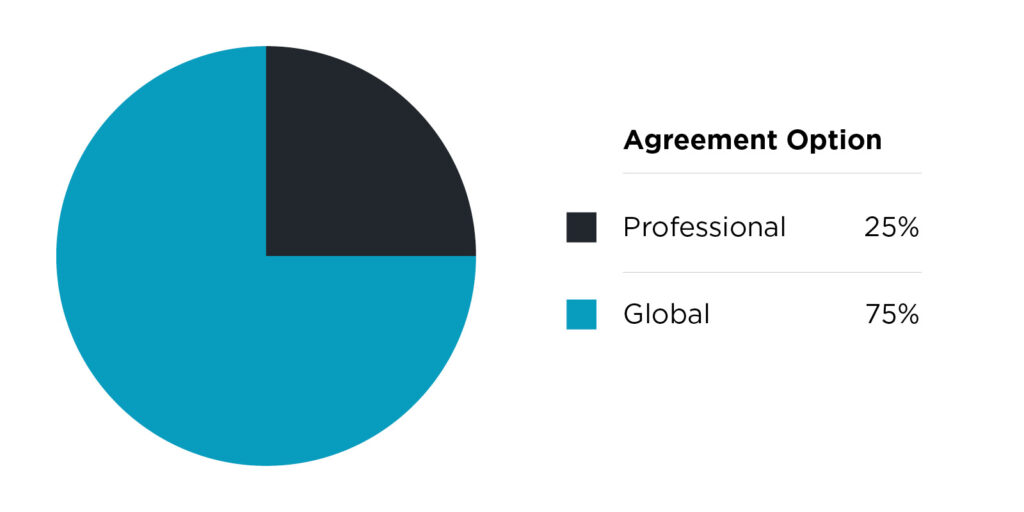
In regard to risk sharing, ACO REACH gives approved participants two options.
There’s the “professional option,” a lower-risk option with 50% shared savings or shared losses, and primary care capitation payment. Then, there’s the “global option,” a full-risk option with 100% shared savings or shared losses, and either primary care capitation or total cost of care capitation.
As of Aug. 25, 110 participants were provisionally accepted into the ACO REACH program for 2023, according to CMS. Another 142 organizations were not selected, marking a 47% acceptance rate.
Over a dozen applicants have withdrawn from participation.
One Medical (Nasdaq: ONEM) and Upward Health are among the approved REACH organizations heading into next year – and both are very focused on executing on the behavioral health front. Both companies are approved under the global option.
“Your standard primary care doctor that is seeing a Medicare patient under the fee-for-service system may want to have a health coach on staff. They may want to have a mental or behavioral health specialist on staff,” Andrew Van Ostrand, head of government affairs at One Medical, told Behavioral Health Business. “They can’t afford to do it because they’re not getting reimbursed.”
Although ACO REACH providers are mainly primary care organizations, the ability to care for a patients’ physical and mental health could lead to cost savings for all parties involved.
“We see 80% of our patients have behavioral health issues of some kind or another,” Glen Moller, CEO of Upward, told BHB. “From an economic perspective, those primary behavioral health patients wind up costing a lot in a physical-medicine sense when they don’t have to. It’s because they’re not getting services. They’re using the ER as a primary care office. They’re not really getting preventive care at the same rate as the rest of the population. Those are problems that we can nip in the bud. What’s interesting is if we were only focused on the behavioral health part of their life, we would miss that.”
The ACO REACH model will start on Jan. 1, 2023, and span four performance years, ending on Dec. 31, 2026.
Different approaches
The ACO REACH model gives participating providers a lot of flexibility on how they implement coordinated care, including behavioral health services.
“I think if you asked 10 people how to define mental and behavioral health care, you’d probably get 10 different answers,” Van Ostrand said. “I think it frankly speaks to the complexity of mental and behavioral health care.”
That means, for ACO REACH organizations and their partners, it’s really important to define parameters and what matters most.
“That’s frankly why you see a lot of the different ACO REACH participants responding differently to mental and behavioral health, and crafting their own programs accordingly,” Van Ostrand continued.
Founded in 2007, One Medical went public in 2020 through a $245 million IPO. The company provides hybrid primary care, as well as behavioral health offerings. In 2021, the company announced it was acquiring Medicare-focused provider Iora Health for $2.1 billion.
The bulk of One Medical’s Medicare business, including its ACO REACH program, falls under the Iora subsidiary. In July, news broke that retail giant Amazon (Nasdaq: AMZN) was buying the company for $3.9 billion.
Iora Health integrates health coaches and behavioral health providers into its model. While ACO REACH only makes up about 40% to 50% of Iora’s patients, Van Ostrand said the program helps the organization find gaps in care and innovate.
“ACO REACH is giving Iora/One medical a capitated payment based on a per patient budget, and they’re basically saying to One Medical/Iora, ‘Here’s what we’re going to give you for this year to make this patient better,’” Van Ostrand said. “It is the nature of that flexible payment that allows us to innovate.”
While behavioral health has been a part of care for Iora Health for some time, Van Ostrand said the ACO REACH model helps encourage collaboration.
“Iora has always had a behavioral health specialist and health care coaching aspect to their care model. They believe – and I believe – that you can’t separate behavioral and mental health, at least not acutely serious behavioral or mental health, from primary care,” Van Ostrand said. “The challenge is that under a non-ACO REACH capitated risk-sharing arrangement, under the legacy fee-for-service model, the fee-for-service model didn’t allow for a collaborative care approach.”
On its end, Upward is taking a different approach to behavioral health. It is looking to help address the barriers individuals with intellectual and developmental disabilities face getting into care.
Upward Health is a primary care practice that integrates behavioral health and social determinants of health into its model. Earlier this month, the company announced the close of a Series B funding round for an undisclosed amount. It’s part of the ACO REACH model sub-sector focused on high needs populations.
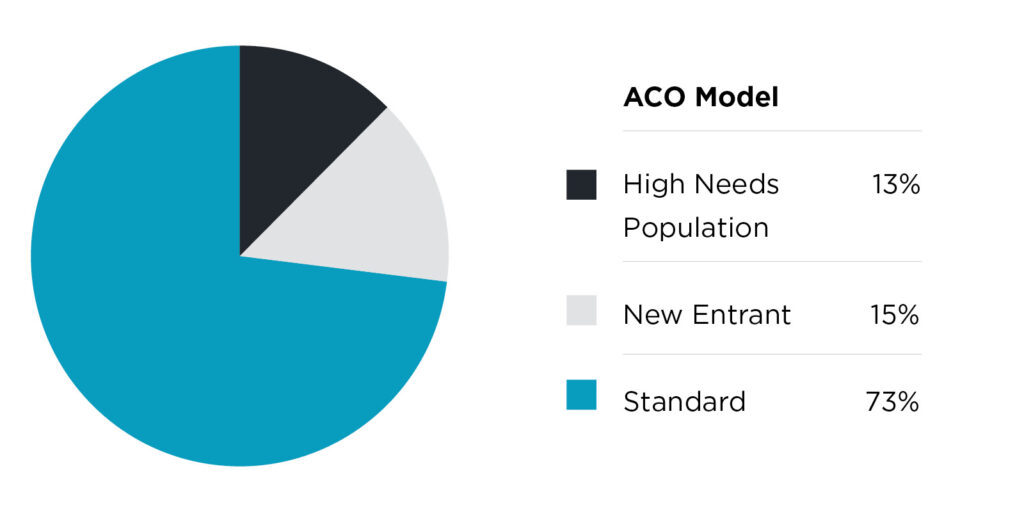
Broadly, the three types of ACO REACH participants are: standard ACOs, new-entrant ACOs and high-needs population ACOs. Besides Upward, examples of the latter include AbsoluteCare ACO, Medallion Health, PCMA Cooperative and several others.
“What we’ve chosen to focus on, in particular with ACO REACH, are individuals with intellectual and developmental disabilities,” Moller said. “If you think about the needs that those individuals have, it’s really hard for them to go get primary care. It’s difficult; they need more time. You can just imagine the problems that we have, or that they have, and so that’s our focus.”
The ACO REACH model could be a way for providers to give patients, particularly those in underserved communities, non-clinical services or support that wouldn’t be reimbursable under a traditional fee-for-service model.
“We have a multidisciplinary team that goes to the patient,” Moller said. “So there’s no bricks and mortar that they ever have to come to. We are literally going to them wherever they are. If there is no home, and they are homeless, we go and meet people wherever they may be.”
Moller noted that this could be particularly helpful for patients needing to get mental health services, where wait times can be very long.
Adding wrap-around services that address social determinants of health and mental health can help the provider save in the long run.
“We don’t necessarily see it as an additive cost,” Van Ostrand said. “We actually see them as all opportunities to reduce higher costs, care somewhere else, or to reduce the inclination of patients, forgoing care that we’ve recommended they receive. Or it’s an opportunity to coordinate care.”
ACO REACH pushback
Direct contracting, and now the ACO REACH model, has faced a wave of criticism from progressive politicians who fear corporate entities could use the program to drive up profits. The House Progressive Caucus has advocated for dissolving the program all together, according to Fierce Healthcare reporting.
The Caucus recommends to “protect seniors’ ability to manage their own care in traditional Medicare by quickly transitioning away from the ACO REACH pilot program, which allows third-party middlemen to manage care without seniors’ full understanding or prior consent, and often through for-profit businesses with incentives to restrict care.”
However, provider organizations have fired back, saying stopping the program could curb innovation.
“We are fiercely opposed to the calls from some that the program should be shut down,” Van Ostrand said. “Because I think what we fear is that if we stop innovating within these alternative payment models, the only alternative is to go back to a medical service system, which has failed patients, I would argue increasingly, for the last three or four decades.”
Currently, the program is designed so that primary care has a more multispecialty approach to care. But it doesn’t necessarily encourage handoffs to other parts of the system, Corbin Petro, CEO and co-founder of Eleanor Health, told BHB.
Yetin the future, partnerships could be a way to help curb this issue.
Eleanor Health is an addiction and mental health care provider focused on building population health and value-based payment models. It has raised about $82 million in funding.
“What I’d love to see is more partnering … in the future. Just a recognition of some of the non-clinical interventions that we know are so important to more vulnerable patient populations,” Petro said. “I think for us, something like 70% of our interventions are not fee-for-service reimbursable. But we do them because it’s right for the patient, and it gets the superior outcomes. That is our North Star.”



