“That’s just the way they are, and speaking to a shrink is not going to help them.”
Over the past several years, there has been a mounting effort in the U.S. to better integrate behavioral health services into nearly every facet of health care, starting with primary care. Despite this focus, behavioral health often remains a missing piece of the puzzle when caring for individuals with intellectual or developmental disabilities (IDDs).
Major misconceptions about the benefits of behavioral health services, such as mental health counseling, are part of the problem, according to Kiley Ritt, manager of behavioral health service and support at the Ohio-based nonprofit Koinonia.
“That [previous] sentence was said to me, and it’s a sticking point that’s … very incorrect,” Ritt said at the 2023 ANCOR Annual Conference. “The idea that someone is the way they are, and that change is not possible, is pretty defeating. Not only for individuals, but for parents – and for staff.”
Founded in 1974, Koinonia provides whole-person care for people with IDDs and other complex conditions in Northeast Ohio. Its offerings include residential, adult day and career services, along with behavioral and mental health care.
Koinonia provides those services to more than 350 clients and families via its staff of about 300 professionals. Since 2021, the nonprofit has been working to be at the forefront of better integrating behavioral health and IDD services, according to CFO and COO Ryan Wood.
“We focus primarily on providing treatment internally, through counseling, as well as behavioral supports,” Wood said at the ANCOR event. “And then we do care management for medication administration, etc.”
Addressing an important need
There is a clear need for integrating behavioral health care into IDD treatment models, with conditions such as anxiety disorders and substance use disorders (SUDs) relatively common among individuals with IDDs.
“Research has indicated that individuals with I/DD may experience a greater prevalence of behavioral health conditions – mental health and substance use disorders – than the
general population,” the U.S. Government Accountability Office (GAO) noted in a recent report.
In putting its report together, GAO reviewed Medicaid data for six states. The government watchdog found that over 45% of Medicaid recipients with IDD enrolled in home- and community-based services (HCBS) programs had an additional health condition, with anxiety, panic disorder and acute conditions frequently observed.
Broadly, mental health conditions were more common than SUDs.
“Of the behavioral health conditions we examined, anxiety disorders, such as panic disorder, were the most common type of behavioral health condition in four of our five selected states with usable diagnosis data: Colorado, Indiana, Oklahoma and South Dakota,” GAO explained. “In 2019, from 13% to 21% of beneficiaries with I/DD in these states had an anxiety disorder
diagnosis. In Georgia, schizophrenia and other psychotic disorders was the most common type of behavioral health condition, affecting 17% of beneficiaries with I/DD.”
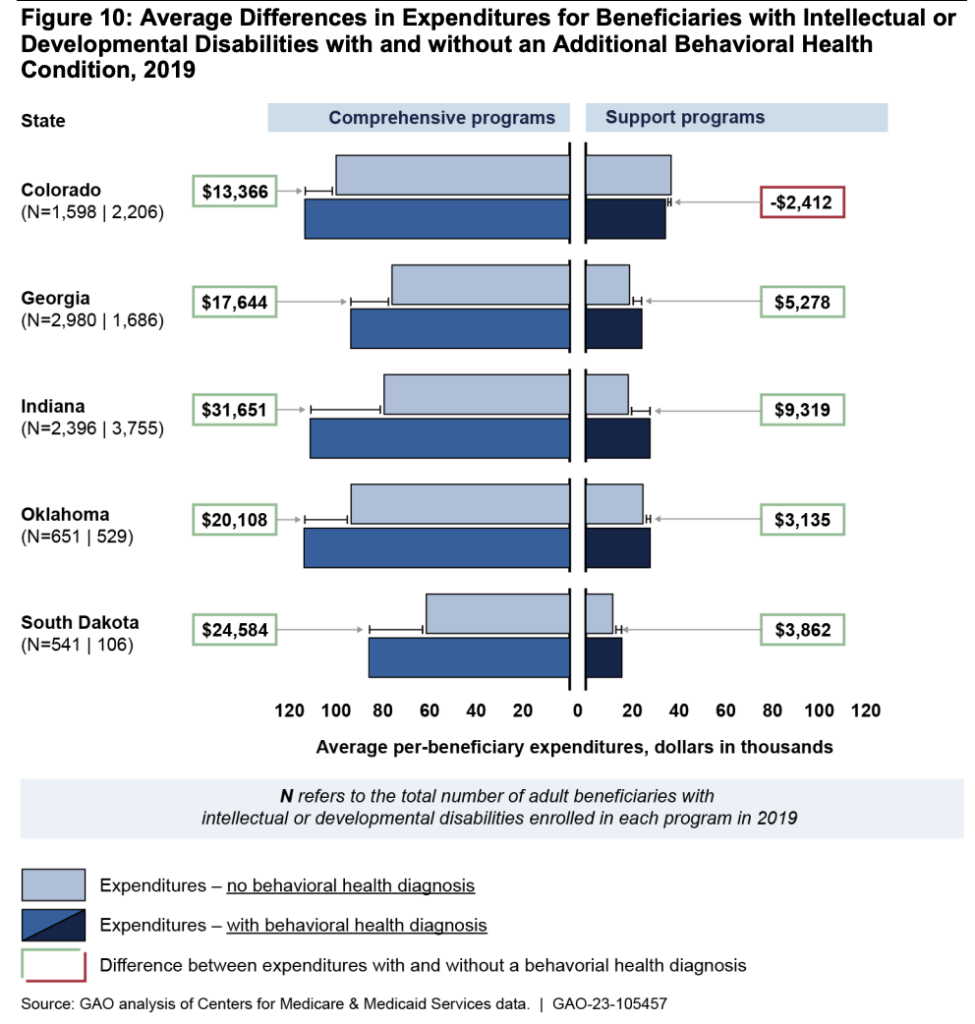
Expenditures were generally higher for Medicaid beneficiaries with IDD who had additional health conditions.
In comprehensive HCBS programs, for instance, expenditures were 13% to 40% higher for beneficiaries with a behavioral health condition than for those without, according to GAO.
Koinonia’s model
Specialized mental health counseling services are the core of Koinonia’s integrated behavioral health strategy. The provider tailors services to the needs of its clients, connecting with them in whatever setting is most convenient, whether that’s their home, workplace, day program, or through telehealth.
“It’s a little like traditional counseling, but it is a bit more specialized. Sessions would look a bit different than you’d expect,” Ritt said. “For any of us who have been in therapy before, you kind of know the drill. But [our services are] a bit more modified, when we are working with those that have a co-occurring IDD diagnosis.”
To illustrate who might benefit from mental health counseling, Ritt offered the example of a client, “John,” whose mom recently passed away. John needed help processing his feelings, but had been denied traditional mental health counseling in the past because of communication barriers.
Koinonia received a referral for John and developed a plan that worked well for him, Ritt said.
“John speaks with a very heavy stutter, and so the counselor said that it was not something that he could continue with, because he wasn’t getting enough accomplished in a traditional session,” he explained. “John was excluded from services. We were able to work with John because he’s excellent at typing. Excellent on the computer. And so we actually sit down, and he kind of types out what he feels, and what he’d like to communicate to me. That has worked really well.”
In cases where mental health counseling isn’t the answer, at least at first, Koinonia offers behavioral supports. Those services, which can be delivered on a short- or long-term basis, often look at medical and environmental reasons behind clients’ behaviors.
Success is largely dependent on collaboration across clients’ care teams, Woods said.
“Beyond the nursing team, it’s really important to have strong pharmacy support and strong medical support,” he said. “Because sometimes, you’ll get a lot of nuanced interactions.”
Neither Woods nor Ritt said how many of Koinonia’s clients use the provider’s mental health and behavioral health services. They did say it was “a large number,” adding that it’d be even greater if there weren’t clinician-capacity constraints.
Challenges to behavioral health-IDD integration
There are numerous challenges to integrating behavioral health services into IDD models.
Toward the top of that list is reimbursement, as not all states reimburse for services the same way. Being in Ohio, Koinonia can have all of its IDD diagnoses count under behavioral health billing, Woods said, noting that grant funding has also been critical.
“We’ve gotten several hundreds of grant dollars that have helped to support this work,” he said. “But certainly, as the field is very much in its … adolescence in this cross-section, that will be an ongoing conversation, especially as we try to scale and continue to evolve the process.”
Finding mental health counselors with training in IDD is likewise difficult.
“When you look at the counseling programs, the educational programs that are out there, there’s not a big section on IDD,” Woods said. “Maybe it’s a chapter, maybe it’s a paragraph. So you’re not seeing a lot of folks come out into the field with a lot of experience.”
The concept of confidentiality is a challenge, too.
When Ritt sees new clients, he’ll frequently have to assure them that their conversations will stay between them “three or four times” because IDD care plans typically have ample communication between all parties involved.
“Confidentiality is a brand new concept for the majority of the folks that we serve. Even the doctors that they see don’t always adhere to the confidentiality that they should,” Ritt said. “So that’s a big part of the initial conversation with new clients.”


